Polycystic ovary syndrome (often called PCOS) is a hormonal disorder that occurs in women during their reproductive years. While research is ongoing, doctors estimate that anywhere between 10-15% of reproductive age women (those who have had their period but not started menopause) have PCOS. Of women who have chronic irregular periods, nearly 90% have PCOS.
Dr. Erin Stone, a gynecologist at Tryon Medical Partners, explains the signs of PCOS, a condition that, while chronic, can be treated and allow one to live a healthy life largely free of disruption.
What are the signs of PCOS and how is it diagnosed?
There are often three telltale signs of those experiencing PCOS:
- Menstrual irregularities (clinically referred to as ovulatory dysfunction): This typically includes frequently missed periods, irregular heavy bleeding during periods or frequently light periods. “Your menstrual cycle is a vital sign that, when disrupted, can point to a larger issue,” Dr. Stone says. “For example, if you’re only having six cycles over the past 12 months, that is a red flag.” With PCOS, your body doesn’t release an egg every month, which is what causes your period. This leads to heavier periods in the months where you do have a period, as the uterine lining has built up for a longer period of time.
- Excessive acne, hair growth or loss, and weight gain (caused by hyperadrenalism): With this condition, the body’s adrenal glands produce excess hormones, causing excessive acne, hair growth and specific types of hair loss. Hyperadrenalism can also lead to weight gain, obesity and resistance to insulin (resulting in many with PCOS being diagnosed as prediabetes).
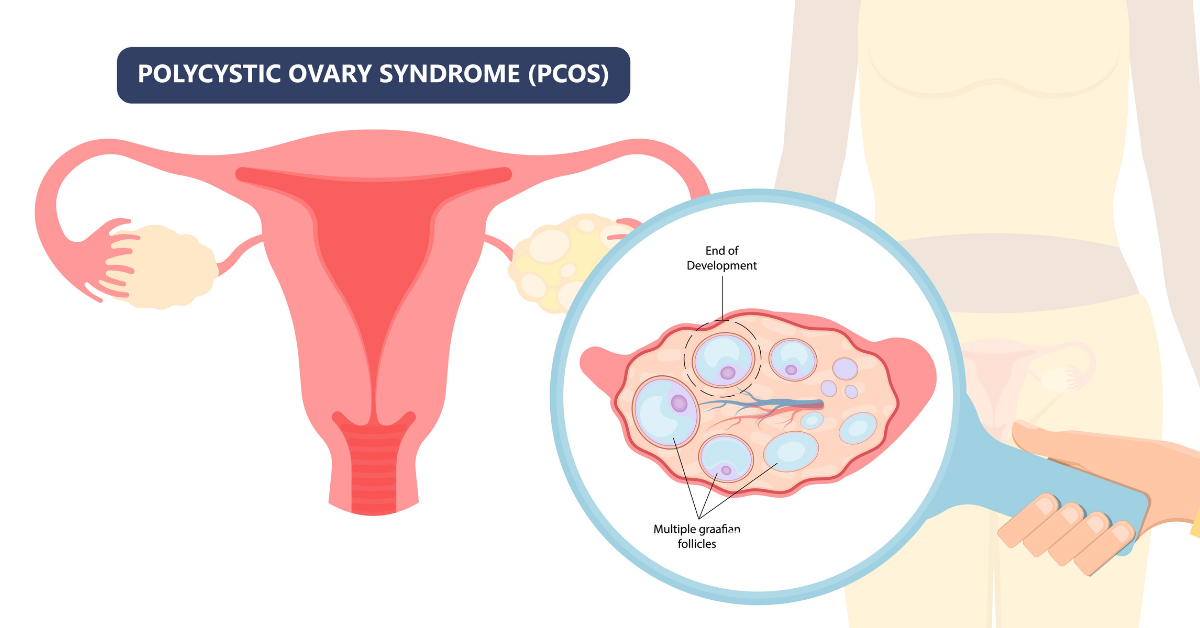
- Tiny cysts on your ovaries (clinically referred to as a polycystic ovary).
Is PCOS a genetic condition?
In some cases, PCOS can be genetic, but that is not always true. Dr. Stone notes that PCOS requires a clinical diagnosis (made by your doctor after reviewing your symptoms and health history), and cannot be diagnosed using laboratory tests or ultrasounds. Before settling on a diagnosis of PCOS, your doctor will also want to rule out thyroid issues, hyperprolactinemia and premature ovarian failure.
When she diagnoses a patient, “I look at the big picture of the patient, rather than just one test,” Dr. Stone says.
How does PCOS impact different patient populations?
Dr. Stone flags that she typically sees three distinct groups of patients who have PCOS and works with them to address issues unique to their diagnosis and life stage. Regardless of the stage that you might fall in upon a PCOS diagnosis, many of these difficulties can be addressed by a combination of lifestyle changes and medication, so don’t be discouraged.
- Adolescents: Dr. Stone recommends that adolescent patients be checked for PCOS when they have missed having their period consistency for a year or two following their first period, flagging that PCOS can often be difficult to face when you’re going through what are already complicated years. Dr. Stone makes sure to help these patients get their PCOS symptoms under control to help curb weight gain, acne, hair growth or loss, and heavy bleeding that can impact their school day. Dr. Stone also makes sure to keep note of when she sees patients developing depression and self-esteem issues as a result of PCOS symptoms. “For patients, including teenagers, PCOS requires a team-based approach,” Dr. Stone says, as oftentimes several health care providers are involved in their care, including mental health providers, dermatologists, endocrinologists, nutritionists and a patient’s pediatrician.
- Patients trying to get pregnant: PCOS does increase risk of fertility issues, as patients do not ovulate and the lining of the uterus is not as favorable to pregnancy in a PCOS patient when compared with someone who doesn’t have the condition. Dr. Stone helps walk patients through potential fertility challenges, and also informs patients that once they are pregnant, they are at a higher risk of gestational diabetes and preeclampsia.
- Patients close to beginning menopause: Dr. Stone likes to alert patients with PCOS who are nearing the end of their reproductive years to keep a special eye on their risk for endometrial cancer, which comes as a result of thicker uterine lining in the body due to PCOS.
What are my treatment options?
Happily, medications and lifestyle change are both very effective at helping patients with PCOS live a healthy, symptom-free life.
“PCOS is chronic, but it’s treatable,” Dr. Stone says. “If you can fix your vital sign (your period), then you are fixing the whole problem.”
Overall, lifestyle modifications can make a big difference on PCOS symptoms, with a main focus on exercise and a diet low in carb-heavy foods. Because PCOS can lead to weight gain and insulin resistance, reducing carb intake can help dramatically with weight loss, which can encourage your ovaries to start functioning regularly again. Consistent exercise, including 40 minutes of cardio activity three to four times a week, can also aid in weight loss.
In addition to lifestyle changes, there are several medications Dr. Stone prescribes patients. First and foremost, Dr. Stone recommends some type of hormonal suppression, such as a birth control pill that has both estrogen and progesterone, which helps keep the uterine lining thin. She also prescribes spironolactone to assist with acne and hair growth. Metformin, an insulin resistance-fighting medication, helps patients thin their uterine lining and ovulate if they are having difficulty getting pregnant.
Is there anything else I should be aware of?
While weight gain and obesity tend to be symptoms of PCOS, Dr. Stone flags that women who are underweight or a normal weight can still have PCOS, as issues with ovulatory dysfunction are the number one sign. Doctors estimate that 20% of PCOS patients are underweight or normal weight, so don’t wait to speak with your doctor if you are concerned that you might meet the other criteria of PCOS.

